
Exhibit 99.1

MONSIE Living with RDEB Corporate Presentation August 2019
Safe Harbor Statement This presentation contains certain statements that may be forward - looking within the meaning of Section 27 a of the Securities Act of 1933 , as amended, including statements relating to the product portfolio and pipeline and clinical programs of the company, the market opportunities for all of the company’s products and product candidates, and the company’s goals and objectives . These statements are subject to numerous risks and uncertainties, including but not limited to the risks detailed in the Company’s Annual Report on Form 10 - K for the year ended December 31 , 2018 , and other reports filed by the company with the Securities and Exchange Commission . This presentation does not constitute an offer or invitation for the sale or purchase of securities or to engage in any other transaction with Abeona Therapeutics or its affiliates . The information in this presentation is not targeted at the residents of any particular country or jurisdiction and is not intended for distribution to, or use by, any person in any jurisdiction or country where such distribution or use would be contrary to local laws or regulations . The Company undertakes no obligations to make any revisions to the forward - looking statements contained in this presentation or to update them to reflect events or circumstances occurring after the date of this presentation, whether as a result of new information, future developments or otherwise . 2
• Pivotal Phase 3 preparation underway in severe form of Epidermolysis Bullosa (EB) • Ongoing Phase 1/2 clinical trials in MPS IIIA and MPS IIIB • Additional programs approaching the clinic in Batten disease (CLN1 and CLN3) • Next generation AIM™ AAV vector platform with in vivo proof of concept data in cystic fibrosis, retinal disorders, Pompe’s and Fabry’s • GMP facility established in Cleveland - Seamless transition from concept - to - commercial across multiple modalities - Quality systems and staff in place to support EB and AAV programs Abeona: A Fully - Integrated Gene & Cell Therapy Company 3
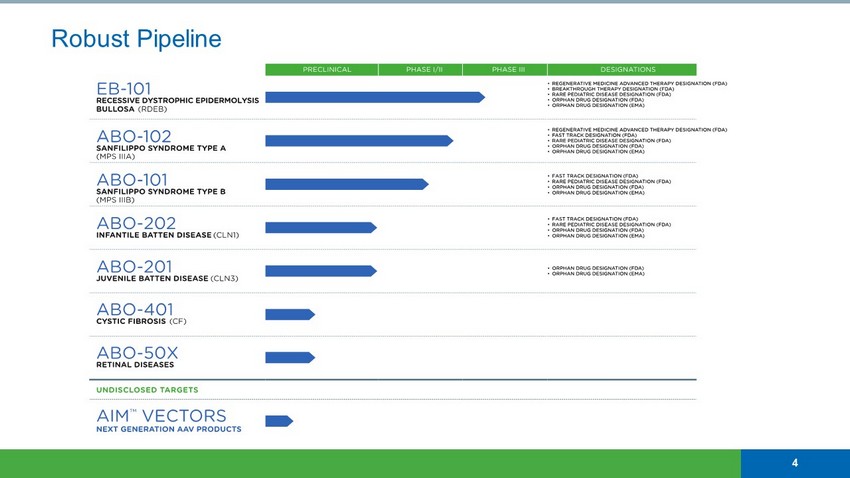
Robust Pipeline 4
RDEB Clinical Program EB - 101 Orphan Drug Designation (FDA) ✓ Orphan Drug Designation (EU) ✓ Rare Pediatric Disease Designation (FDA) ✓ Breakthrough Therapy Designation (FDA) ✓ Regenerative Medicine Advanced Therapy Designation (FDA) ✓
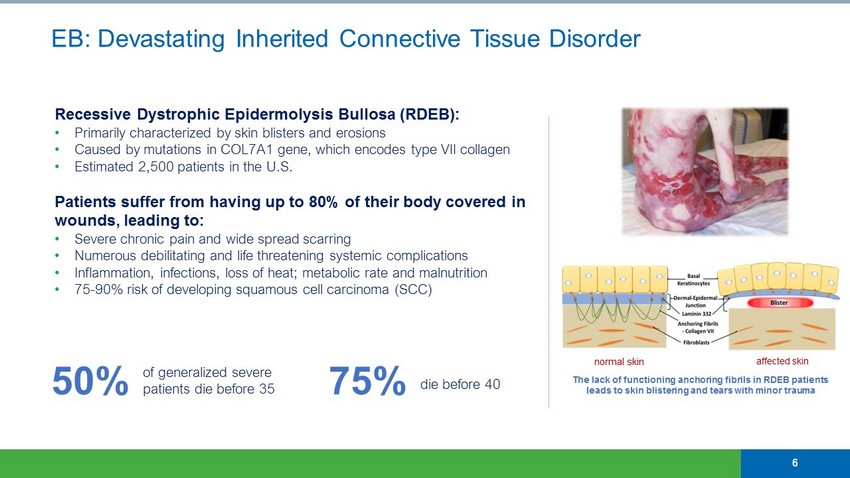
Recessive Dystrophic Epidermolysis Bullosa (RDEB): • Primarily characterized by skin blisters and erosions • Caused by mutations in COL7A1 gene, which encodes type VII collagen • Estimated 2,500 patients in the U.S. Patients suffer from having up to 80% of their body covered in wounds, leading to: • Severe chronic pain and wide spread scarring • Numerous debilitating and life threatening systemic complications • Inflammation, infections, loss of heat; metabolic rate and malnutrition • 75 - 90% risk of developing squamous cell carcinoma (SCC) EB: Devastating Inherited Connective Tissue Disorder 6 50% of generalized severe patients die before 35 75% die before 40 The lack of functioning anchoring fibrils in RDEB patients leads to skin blistering and tears with minor trauma normal skin affected skin
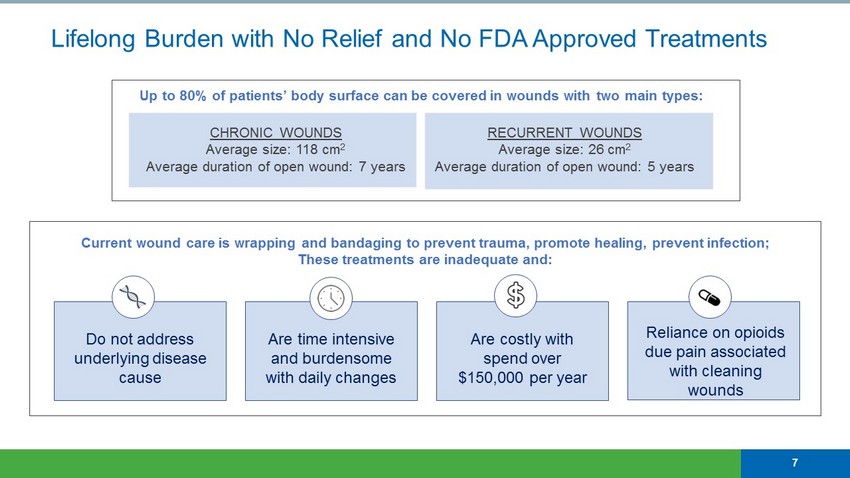
Lifelong Burden with No Relief and No FDA Approved Treatments 7 CHRONIC WOUNDS Average size: 118 cm 2 Average duration of open wound: 7 years RECURRENT WOUNDS Average size: 26 cm 2 Average duration of open wound: 5 years Up to 80% of patients’ body surface can be covered in wounds with two main types: Current wound care is wrapping and bandaging to prevent trauma, promote healing, prevent infection; These treatments are inadequate and: Do not address underlying disease cause Are time intensive and burdensome with daily changes Reliance on opioids due pain associated with cleaning wounds Are costly with spend over $150,000 per year
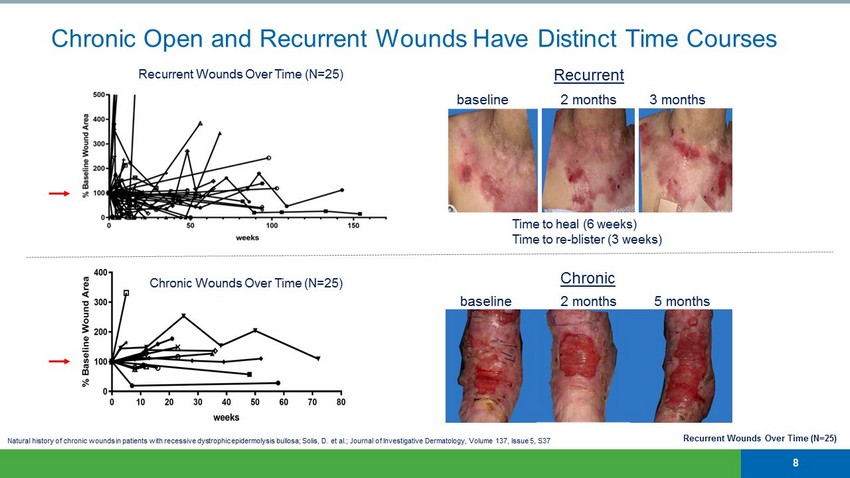
Recurrent Wounds Over Time (N=25) Chronic Open and Recurrent Wounds Have Distinct Time Courses Time to heal (6 weeks) Time to re - blister (3 weeks) baseline 2 months 5 months baseline 2 months 3 months Chronic Recurrent Recurrent Wounds Over Time (N=25) Chronic Wounds Over Time (N=25) 8 Natural history of chronic wounds in patients with recessive dystrophic epidermolysis bullosa; Solis, D. et al.; Journal of I nve stigative Dermatology, Volume 137, Issue 5, S37
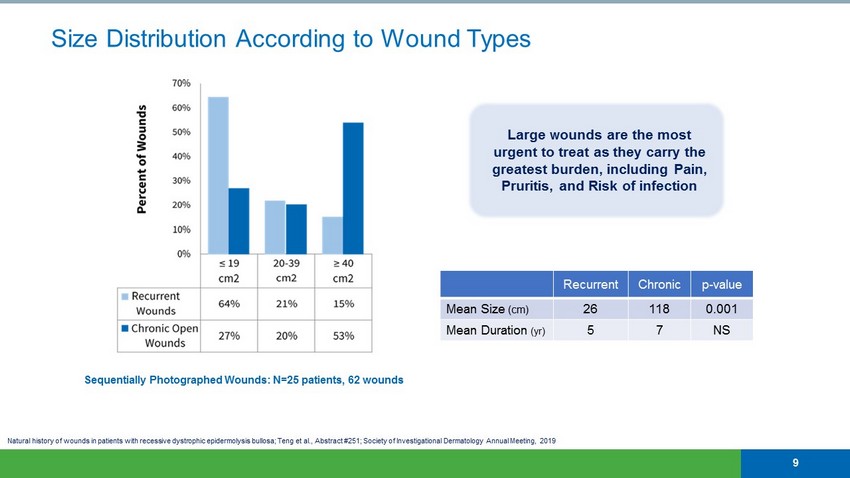
Size Distribution According to Wound Types 9 Large wounds are the most urgent to treat as they carry the greatest burden, including Pain, Pruritis, and Risk of infection Recurrent Chronic p - value Mean Size (cm) 26 118 0.001 Mean Duration ( yr ) 5 7 NS Sequentially Photographed Wounds: N=25 patients, 62 wounds Natural history of wounds in patients with recessive dystrophic epidermolysis bullosa; Teng et al., Abstract #251; Society of In vestigational Dermatology Annual Meeting, 2019
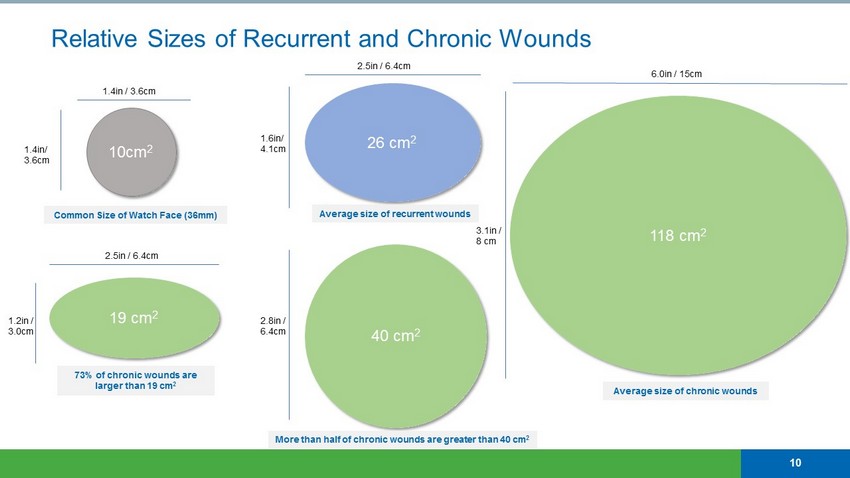
Relative Sizes of Recurrent and Chronic Wounds 10cm 2 19 cm 2 2.5in / 6.4cm 1.4in / 3.6cm Common Size of Watch Face (36mm) 73% of chronic wounds are larger than 19 cm 2 26 cm 2 2.5in / 6.4cm Average size of recurrent wounds 40 cm 2 More than half of chronic wounds are greater than 40 cm 2 118 cm 2 1.6in/ 4.1cm 2.8in / 6.4cm 1.4in/ 3.6cm 1.2in / 3.0cm 3.1in / 8 cm 6.0in / 15cm Average size of chronic wounds 10
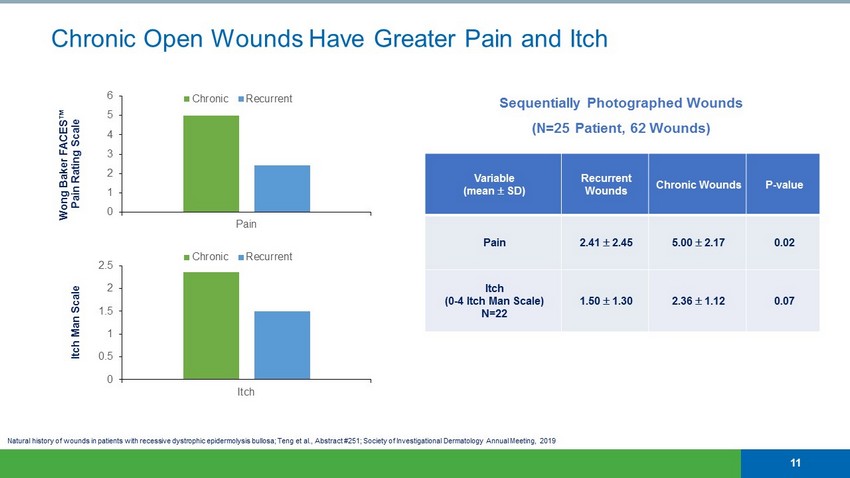
Natural history of wounds in patients with recessive dystrophic epidermolysis bullosa; Teng et al., Abstract #251; Society of In vestigational Dermatology Annual Meeting, 2019 Sequentially Photographed Wounds (N=25 Patient, 62 Wounds) 0 1 2 3 4 5 6 Pain Chronic Recurrent Wong Baker FACES™ Pain Rating Scale Itch Man Scale Chronic Open Wounds Have Greater Pain and Itch 0 0.5 1 1.5 2 2.5 Itch Chronic Recurrent Variable (mean SD) Recurrent Wounds Chronic Wounds P - value Pain 2.41 2.45 5.00 2.17 0.02 Itch (0 - 4 Itch Man Scale) N=22 1.50 1.30 2.36 1.12 0.07 11
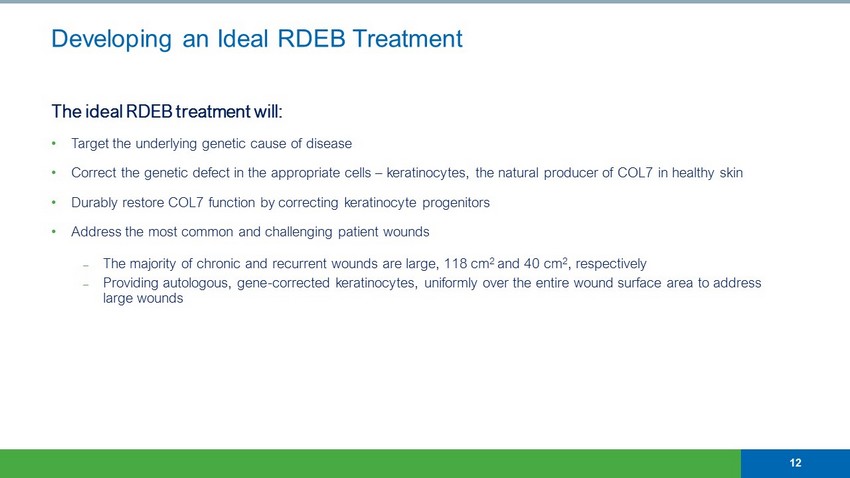
Developing an Ideal RDEB Treatment The ideal RDEB treatment will: • Target the underlying genetic cause of disease • Correct the genetic defect in the appropriate cells – keratinocytes, the natural producer of COL7 in healthy skin • Durably restore COL7 function by correcting keratinocyte progenitors • Address the most common and challenging patient wounds ⎼ The majority of chronic and recurrent wounds are large, 118 cm 2 and 40 cm 2 , respectively ⎼ Providing autologous, gene - corrected keratinocytes, uniformly over the entire wound surface area to address large wounds 12
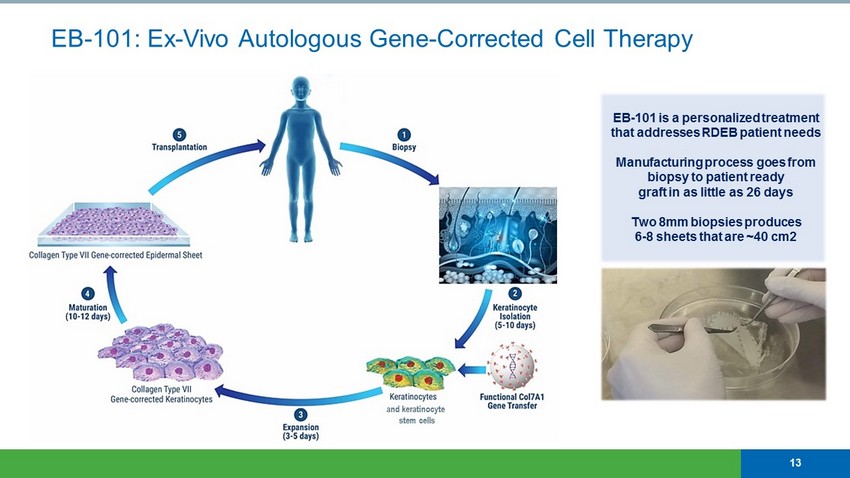
EB - 101: Ex - Vivo Autologous Gene - Corrected Cell Therapy 13 EB - 101 is a personalized treatment that addresses RDEB patient needs Manufacturing process goes from biopsy to patient ready graft in as little as 26 days Two 8mm biopsies produces 6 - 8 sheets that are ~40 cm2 and keratinocyte stem cells
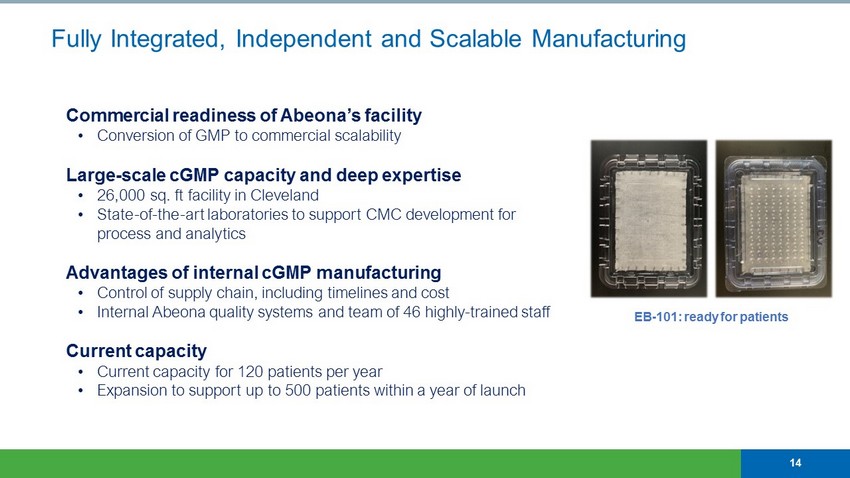
EB - 101: ready for patients Fully Integrated, Independent and Scalable Manufacturing 14 Commercial readiness of Abeona’s facility • Conversion of GMP to commercial scalability Large - scale cGMP capacity and deep expertise • 26,000 sq. ft facility in Cleveland • State - of - the - art laboratories to support CMC development for process and analytics Advantages of internal cGMP manufacturing • Control of supply chain, including timelines and cost • Internal Abeona quality systems and team of 46 highly - trained staff Current capacity • Current capacity for 120 patients per year • Expansion to support up to 500 patients within a year of launch
Study Description A Phase I/IIa Single Center Trial of Gene Transfer for Recessive Dystrophic Epidermolysis Bullosa (RDEB) using EB - 101 for autologous tissue transplantation Trial Design • Open - label, interventional study • Seven patients with RDEB (ages 18 to 45 years) • Follow - up visits at 1 month - 12 months, then yearly in a long - term follow - up protocol until year 5 EB - 101 Phase I/IIa Trial – Addressed Complex and Challenging Wounds Phase I/IIa trial addressed wounds of increasing severity and complexity • Abeona pushed to treat challenging wounds that were representative of those most troublesome for the RDEB population • Learnings from program de - risked Phase 3, providing essential guidance for future wound treatment Abeona believes all wounds, regardless of size or duration of open wound, can be addressed with EB - 101 15
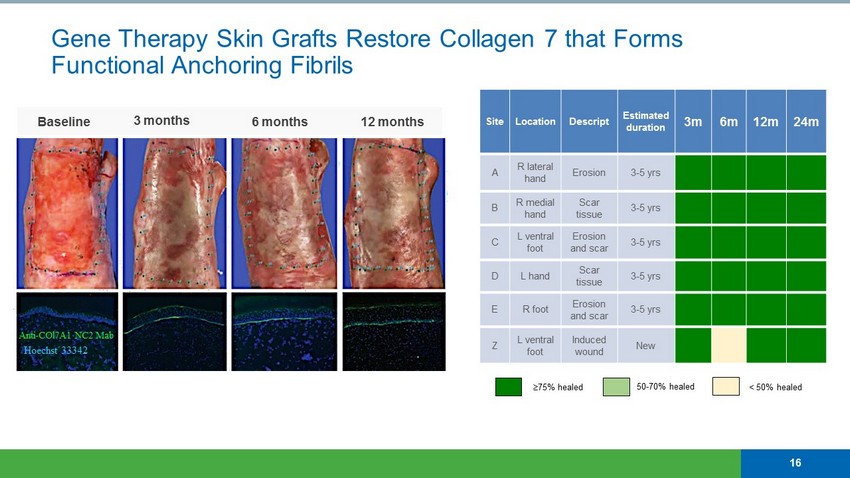
Site Location Descript Estimated duration 3m 6m 12m 24m A R lateral hand Erosion 3 - 5 yrs B R medial hand Scar tissue 3 - 5 yrs C L ventral foot Erosion and scar 3 - 5 yrs D L hand Scar tissue 3 - 5 yrs E R foot Erosion and scar 3 - 5 yrs Z L ventral foot Induced wound New 75% healed 50 - 70 % healed < 50% healed Baseline 3 months 6 months 12 months Gene Therapy Skin Grafts Restore Collagen 7 that Forms Functional Anchoring Fibrils 16 Anti - COl7A1 NC2 Mab Hoechst 33342
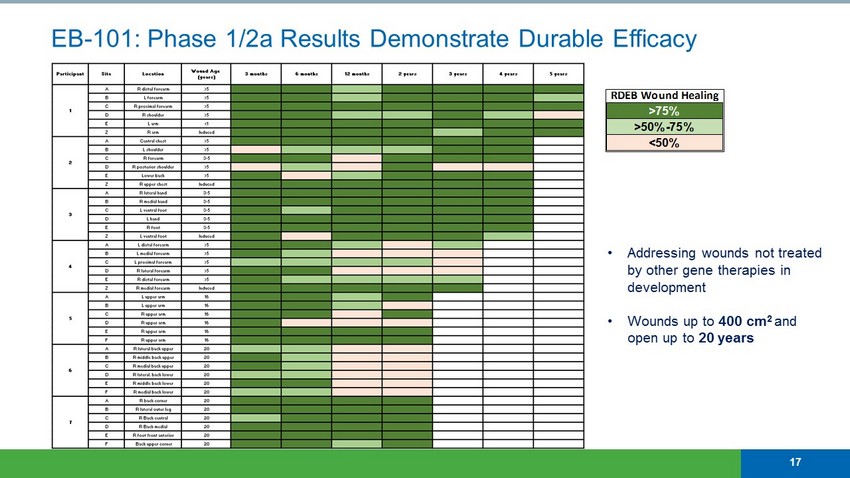
EB - 101: Phase 1/2a Results Demonstrate Durable Efficacy RDEB Wound Healing >75% >50%-75% <50% 17 • Addressing wounds not treated by other gene therapies in development • Wounds up to 400 cm 2 and open up to 20 years
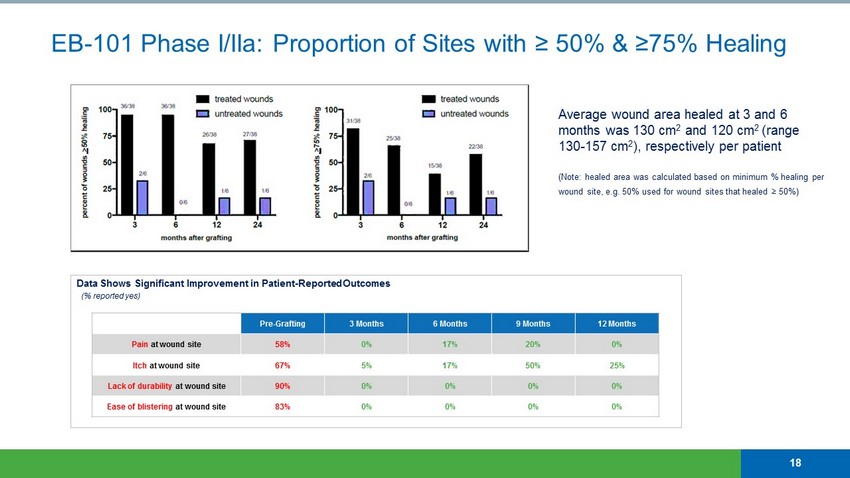
EB - 101 Phase I/IIa: Proportion of Sites with ≥ 50% & ≥75% Healing Average wound area healed at 3 and 6 months was 130 cm 2 and 120 cm 2 (range 130 - 157 cm 2 ), respectively per patient (Note: healed area was calculated based on minimum % healing per wound site, e.g. 50% used for wound sites that healed ≥ 50%) 18 Pre - Grafting 3 Months 6 Months 9 Months 12 Months Pain at wound site 58% 0% 17% 20% 0% Itch at wound site 67% 5% 17% 50% 25% Lack of durability at wound site 90% 0% 0% 0% 0% Ease of blistering at wound site 83% 0% 0% 0% 0% Data Shows Significant Improvement in Patient - Reported Outcomes (% reported yes)

EB - 101 Summary and Anticipated Next Steps Successful Phase 1/2 • Favorable safety profile with no product - related SAEs to date • Significant and durable wound healing, with up to 5 years of follow - up • Continuous type VII collagen expression 2+ years post treatment Established GMP manufacturing capability at Abeona • Manufacture both clinical and commercial product in Cleveland • Scalable capacity to support commercial launch VIITAL ™ : Phase 3 Trial • Regulatory CMC review Q3 2019 • First patient expected to enroll Q4 2019 19

MPS III Clinical Programs ABO - 102* ABO - 101 Orphan Drug Designation (FDA) ✓ Orphan Drug Designation (EU) ✓ Rare Pediatric Disease Designation (FDA) ✓ Fast Track Designation (FDA) ✓ Regenerative Medicine Advanced Therapy Designation* (FDA) ✓
Inherited monogenic disorders causing lysosomal enzyme deficiency • Two most common forms categorized by deficient enzymes: – MPS IIIA (SGSH), MPS IIIB (NAGLU) • Abnormal accumulation of glycosaminoglycans (GAGs; heparan sulfate (HS)) • Loss of speech/vision, cognitive decline, behavioral abnormalities, seizures, sleep disturbances • 70% of children with MPS III do not reach age 18 years No approved treatments available Estimated incidence of 1 in 70,000 births Two ongoing global clinical trials: • ABO - 102 (AAV - SGSH) for MPS IIIA: USA, EU, Australia clinical sites • ABO - 101 (AAV - NAGLU) for MPS IIIB: USA and EU clinical sites Cell with lysosome deficiency Normal cell Ongoing Phase 1/2 Clinical Trials for Sanfilippo Syndrome (MPS III) 21
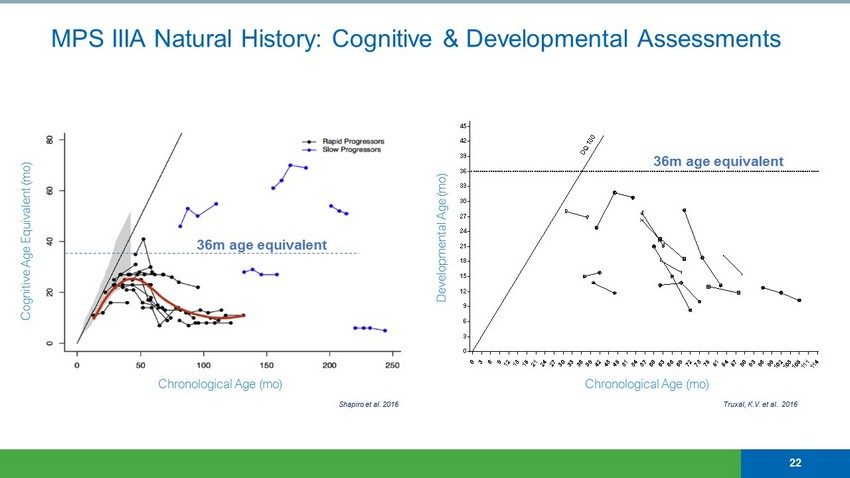
MPS IIIA Natural History: Cognitive & Developmental Assessments 22 Chronological Age (mo) Cognitive Age Equivalent (mo) Shapiro et al. 2016 0 3 6 9 1 2 1 5 1 8 2 1 2 4 2 7 3 0 3 3 3 6 3 9 4 2 4 5 4 8 5 1 5 4 5 7 6 0 6 3 6 6 6 9 7 2 7 5 7 8 8 1 8 4 8 7 9 0 9 3 9 6 9 9 1 0 2 1 0 5 1 0 8 1 1 1 1 1 4 1 1 7 0 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45 Chronological Age (Month) D e v e l o p m e n t a l A g e ( M o n t h ) D Q 1 0 0 Chronological Age (mo) Developmental Age (mo) Truxal, K.V. et al. 2016 36m age equivalent 36m age equivalent
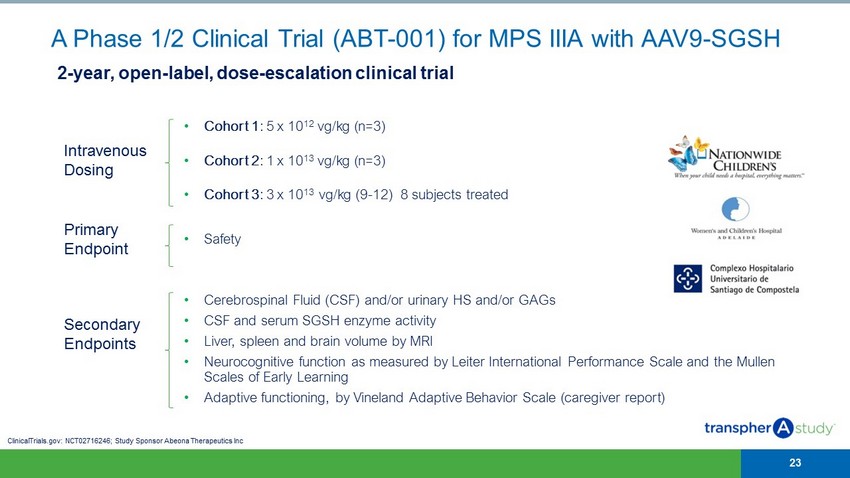
Intravenous Dosing • Cohort 1 : 5 x 10 12 vg/kg (n=3) • Cohort 2 : 1 x 10 13 vg/kg (n=3) • Cohort 3 : 3 x 10 13 vg/kg (9 - 12) 8 subjects treated Primary Endpoint • Safety Secondary Endpoints • Cerebrospinal Fluid (CSF) and/or urinary HS and/or GAGs • CSF and serum SGSH enzyme activity • Liver, spleen and brain volume by MRI • Neurocognitive function as measured by Leiter International Performance Scale and the Mullen Scales of Early Learning • Adaptive functioning, by Vineland Adaptive Behavior Scale (caregiver report) A Phase 1/2 Clinical Trial (ABT - 001) for MPS IIIA with AAV9 - SGSH 23 2 - year, open - label, dose - escalation clinical trial ClinicalTrials.gov: NCT02716246; Study Sponsor Abeona Therapeutics Inc
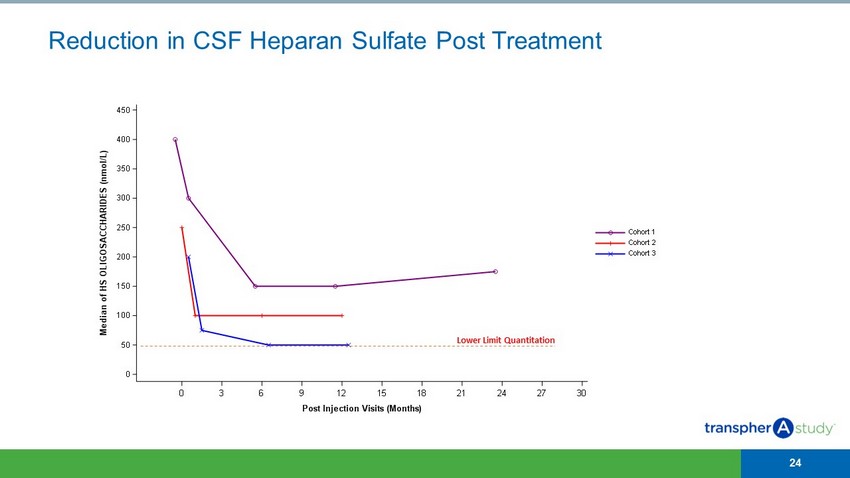
Reduction in CSF Heparan Sulfate Post Treatment 24 0 3 6 9 12 15 18 21 24 27 30 Post Injection Visits (Months) 0 50 100 150 200 250 300 350 400 450 M e d i a n o f H S O L I G O S A C C H A R I D E S ( n m o l / L ) Cohort 3 Cohort 2 Cohort 1 Lower Limit Quantitation
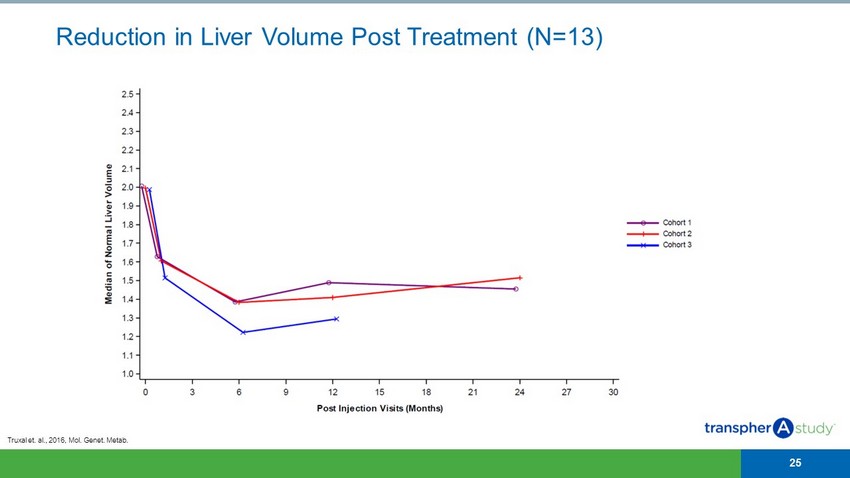
Reduction in Liver Volume Post Treatment (N=13) 25 Truxal et. al., 2016, Mol. Genet. Metab .
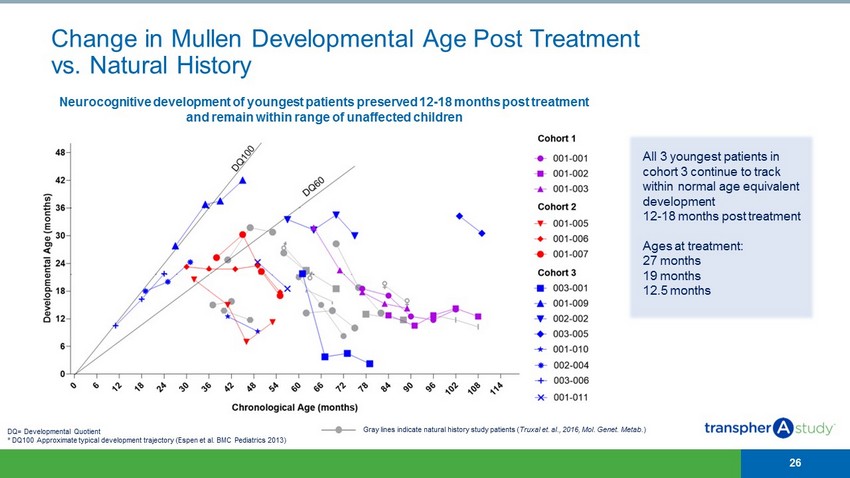
Change in Mullen Developmental Age Post Treatment vs. Natural History 26 Gray lines indicate natural history study patients ( Truxal et. al., 2016, Mol. Genet. Metab . ) All 3 youngest patients in cohort 3 continue to track within normal age equivalent development 12 - 18 months post treatment Ages at treatment: 27 months 19 months 12.5 months Neurocognitive development of youngest patients preserved 12 - 18 months post treatment and remain within range of unaffected children DQ= Developmental Quotient * DQ100 Approximate typical development trajectory ( Espen et al. BMC Pediatrics 2013)
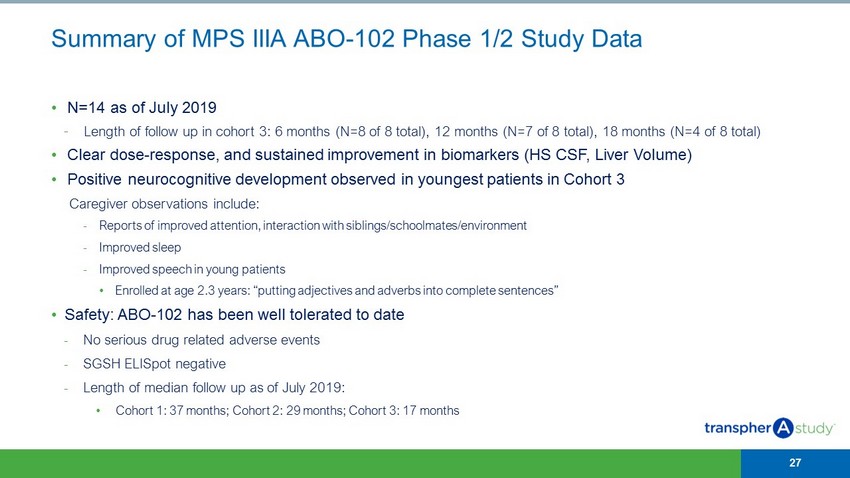
Summary of MPS IIIA ABO - 102 Phase 1/2 Study Data • N=14 as of July 2019 - Length of follow up in cohort 3: 6 months (N=8 of 8 total), 12 months (N=7 of 8 total), 18 months (N=4 of 8 total) • Clear dose - response, and sustained improvement in biomarkers (HS CSF, Liver Volume) • Positive neurocognitive development observed in youngest patients in Cohort 3 Caregiver observations include: - Reports of improved attention, interaction with siblings/schoolmates/environment - Improved sleep - Improved speech in young patients • Enrolled at age 2.3 years: “putting adjectives and adverbs into complete sentences” • Safety: ABO - 102 has been well tolerated to date - No serious drug related adverse events - SGSH ELISpot negative - Length of median follow up as of July 2019: • Cohort 1: 37 months; Cohort 2: 29 months; Cohort 3: 17 months 27
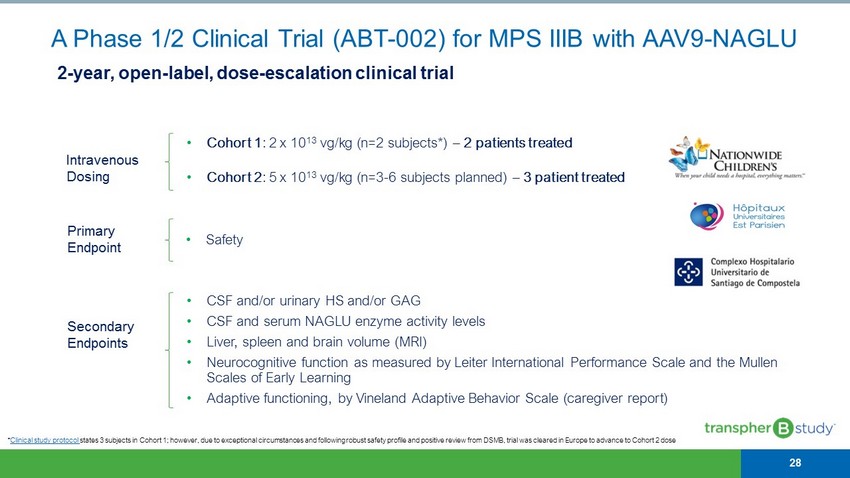
* Clinical study protocol states 3 subjects in Cohort 1; however, due to exceptional circumstances and following robust safety profile and positive rev iew from DSMB, trial was cleared in Europe to advance to Cohort 2 dose Intravenous Dosing • Cohort 1 : 2 x 10 13 vg/kg (n=2 subjects*) – 2 patients treated • Cohort 2 : 5 x 10 13 vg/kg (n=3 - 6 subjects planned) – 3 patient treated Primary Endpoint • Safety Secondary Endpoints • CSF and/or urinary HS and/or GAG • CSF and serum NAGLU enzyme activity levels • Liver, spleen and brain volume (MRI) • Neurocognitive function as measured by Leiter International Performance Scale and the Mullen Scales of Early Learning • Adaptive functioning, by Vineland Adaptive Behavior Scale (caregiver report) A Phase 1/2 Clinical Trial (ABT - 002) for MPS IIIB with AAV9 - NAGLU 28 2 - year, open - label, dose - escalation clinical trial
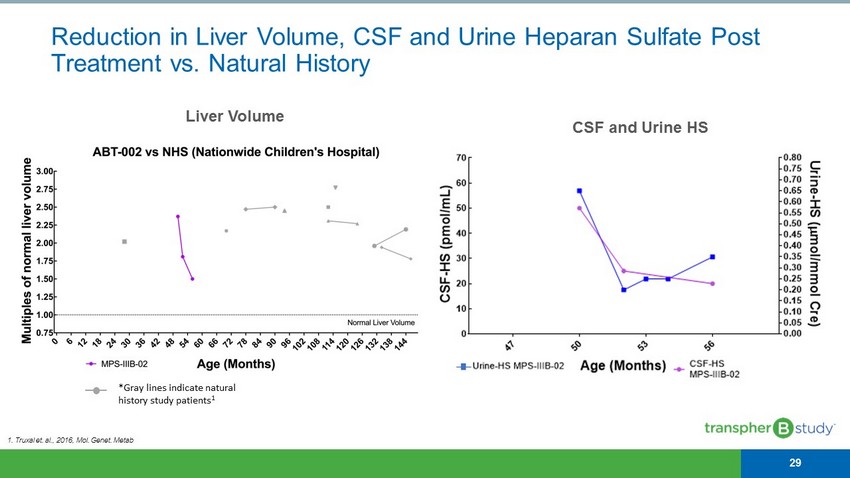
1. Truxal et. al., 2016, Mol. Genet. Metab Liver Volume CSF and Urine HS Reduction in Liver Volume, CSF and Urine Heparan Sulfate Post Treatment vs. Natural History 29 *Gray lines indicate natural history study patients 1
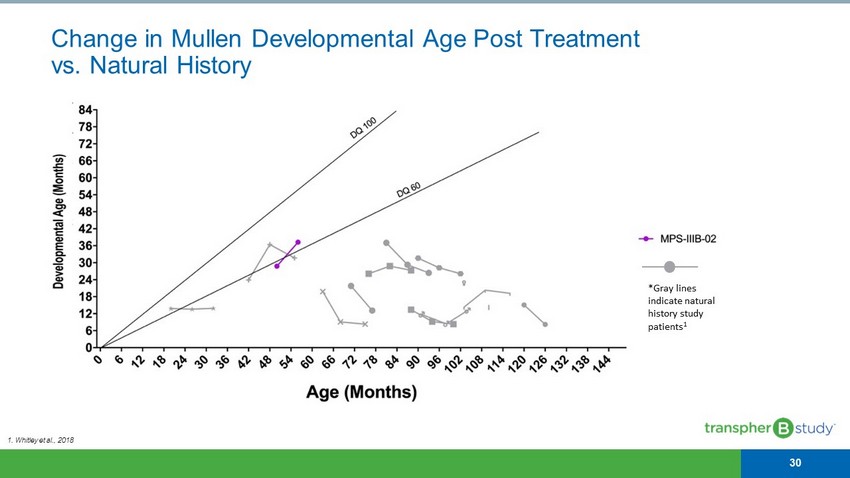
Change in Mullen Developmental Age Post Treatment vs. Natural History 30 *Gray lines indicate natural history study patients 1 1. Whitley et al., 2018

CLN1 (Infantile Batten) Disease ABO - 202 Orphan Drug Designation (FDA) ✓ Orphan Drug Designation (EU) ✓ Rare Pediatric Disease Designation (FDA) ✓ Fast Track Designation (FDA) ✓
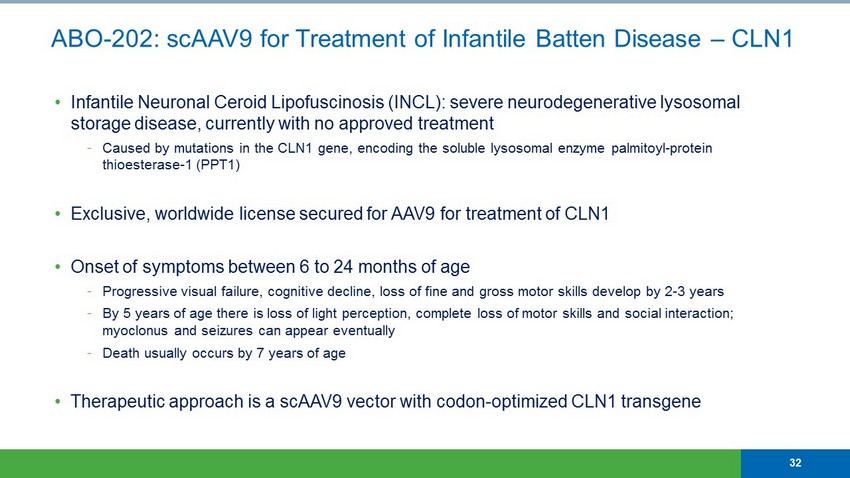
• Infantile Neuronal Ceroid Lipofuscinosis (INCL): severe neurodegenerative lysosomal storage disease, currently with no approved treatment - Caused by mutations in the CLN1 gene, encoding the soluble lysosomal enzyme palmitoyl - protein thioesterase - 1 (PPT1) • Exclusive, worldwide license secured for AAV9 for treatment of CLN1 • Onset of symptoms between 6 to 24 months of age - Progressive visual failure, cognitive decline, loss of fine and gross motor skills develop by 2 - 3 years - By 5 years of age there is loss of light perception, complete loss of motor skills and social interaction; myoclonus and seizures can appear eventually - Death usually occurs by 7 years of age • Therapeutic approach is a scAAV9 vector with codon - optimized CLN1 transgene 32 ABO - 202: scAAV9 for Treatment of Infantile Batten Disease – CLN1
• IND - enabling toxicology and efficacy studies completed ⎻ Strong safety, with no significant toxicology findings in the combination dose escalation study ⎻ Data demonstrated normalized survival, muscle function and cognition • FDA IND clearance received Q2 2019 • Potential Benefits of IT/IV dosing include: - Overcoming IT dose limitations due to volume constraints and bolsters IV doses, especially in older patients - “Double exposure” to the CNS enables broad and distributed coverage • Trial outcomes supported by large, multi - year Natural History Study • World - leading investigators and clinical sites for CLN1 ⎻ University of Rochester and University of Hamburg 33 Steven Gray, Ph.D. - Batten Researcher ABO - 202: Phase 1/2 clinical trial readiness
Next Generation AIM TM AAV Platform
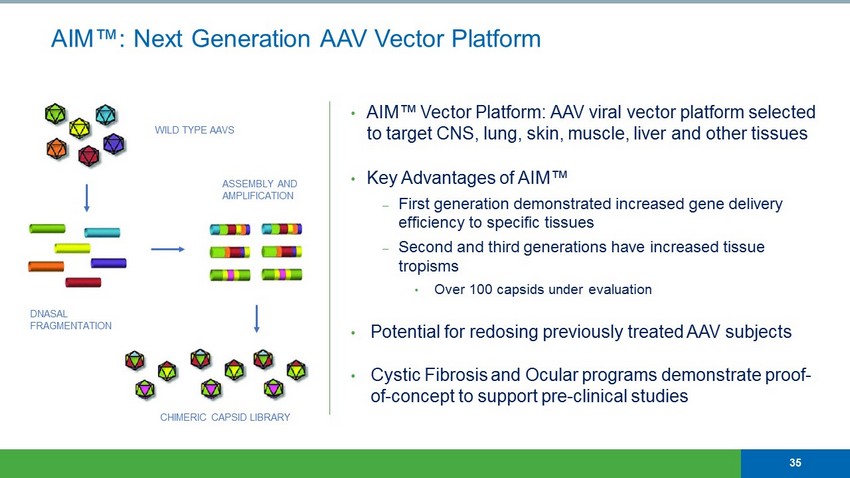
AIM™: Next Generation AAV Vector Platform • AIM™ Vector Platform: AAV viral vector platform selected to target CNS, lung, skin, muscle, liver and other tissues • Key Advantages of AIM™ ⎼ First generation demonstrated increased gene delivery efficiency to specific tissues ⎼ Second and third generations have increased tissue tropisms • Over 100 capsids under evaluation • Potential for redosing previously treated AAV subjects • Cystic Fibrosis and Ocular programs demonstrate proof - of - concept to support pre - clinical studies DNASAL FRAGMENTATION ASSEMBLY AND AMPLIFICATION CHIMERIC CAPSID LIBRARY WILD TYPE AAVS 35

AAV GMP MANUFACTURING
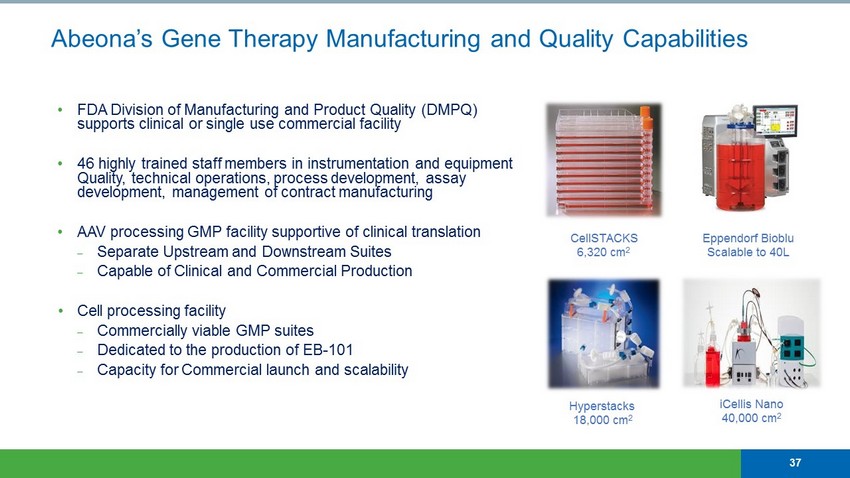
Abeona’s Gene Therapy Manufacturing and Quality Capabilities • FDA Division of Manufacturing and Product Quality (DMPQ) supports clinical or single use commercial facility • 46 highly trained staff members in instrumentation and equipment Quality, technical operations, process development, assay development, management of contract manufacturing • AAV processing GMP facility supportive of clinical translation ⎼ Separate Upstream and Downstream Suites ⎼ Capable of Clinical and Commercial Production • Cell processing facility ⎼ Commercially viable GMP suites ⎼ Dedicated to the production of EB - 101 ⎼ Capacity for Commercial launch and scalability Hyperstacks 18,000 cm 2 Eppendorf Bioblu Scalable to 40L CellSTACKS 6,320 cm 2 iCellis Nano 40,000 cm 2 37

João Siffert, M.D. Chief Executive Officer, Head of R&D, Chief Medical Officer Timothy J. Miller, Ph.D. President, Chief Scientific Officer Christine Silverstein Chief Financial Officer Management Team Max Colao Chief Commercial Officer, Head of Business Development Edward Carr Chief Accounting Officer Edward Sturchio SVP, General Counsel & Corporate Secretary Maria Escolar, M.D. Pittsburgh Children’s Hospital John Cooper, Ph.D. University of California, San Diego Scientific Advisors Jonathan Mink, M.D., Ph.D. University of Rochester Erika Augustine, M.D. University of Rochester Steven Gray, Ph.D. University of Texas Southwestern Kevin Flanigan, M.D. Nationwide Children’s Hospital Juan Ruiz, M.D., Ph.D. Head of European Medical Affairs Victor Paulus, Ph.D. SVP, Regulatory Affairs Jay Bircher SVP, Quality & Technical Operations 38